Ultrasound-Guided Radiofrequency Ablation of Thyroid Nodules
RADIOFREQUENCY ABLATION - GETTYSBURG, PA
A LEADING EDGE NON-SURGICAL TREATMENT OF THYROID NODULES
Our brains, our hearts, our digestive and metabolic systems function normally with the help of one small gland: the thyroid gland.
Nodules on the thyroid gland, however common, can interfere with the proper functioning of the thyroid gland; Benign nodules can cause swallowing difficulty, excessive hormone production, and pressure symptoms within the neck.
Most thyroid nodules are benign and do not require any specific treatment. The small percentage of thyroid nodules that are malignant are generally treated with surgery and additional therapies in attempt to cure the underlying disease and prevent recurrence.
Some benign thyroid nodules do grow to the point of causing cosmetic concerns or compressive symptoms on surrounding structures in the neck requiring treatment. Typically this treatment has involved surgery.
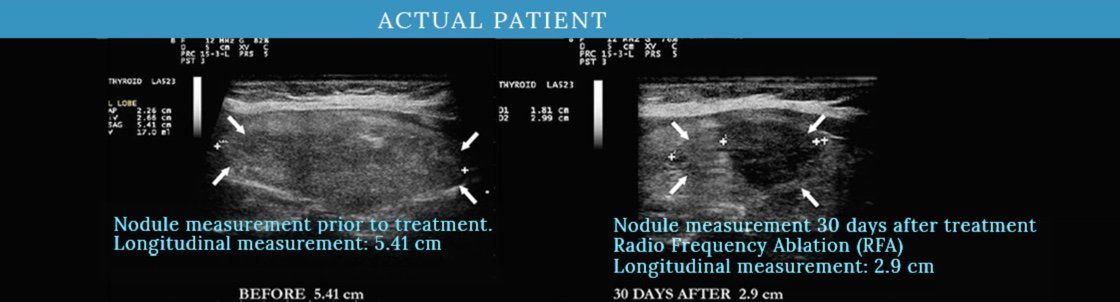
Radiofrequency ablation (RFA)
is a minimally invasive percutaneous treatment of benign solid thyroid nodules that results in thermal tissue damage and fibrosis leading to shrinkage of the nodule. Clinical studies in Europe and Asia have demonstrated a durable 50-80 percent reduction in the size of thyroid nodules treated with RFA.
Until recently, available technology for performance of this procedure required a patient to be placed under general anesthesia to have the treatment performed. The FDA has recently approved newer technology that allows RFA to be performed as an outpatient office procedure
under local anesthesia.
WHAT ARE TRADITIONAL TREATMENTS?
Traditional treatment options include surgery, radioactive iodine therapy and/or medication.
WHAT ARE THE DRAWBACKS OF TRADITIONAL TREATMENTS?
All have drawbacks.
Surgery requires general anesthesia, hospitalization, painful recovery time, and permanent scarring.
Radioactive iodine therapy can require hospitalization in an isolation room. Children can not be exposed to the patient for several days after the treatment. Side effects include nausea, swelling and tenderness in the neck area, dry mouth, and a persistent metallic taste.
Thyroid hormone medication involves continual monitoring and adjustment by the physician, and regular blood tests to determine proper dosage. The process is lifelong.
IS THERE AN EASIER OPTION?
Radiofrequency ablation
is an easier option. RFA is an FDA approved non-surgical procedure
that shrinks the nodules without compromising thyroid function and helps avoid long recovery times of thyroid surgery.
FROM RGS HEALTHCARE:
Please contact Randi Bucher for information rbucher@adamsendocrinology.com.
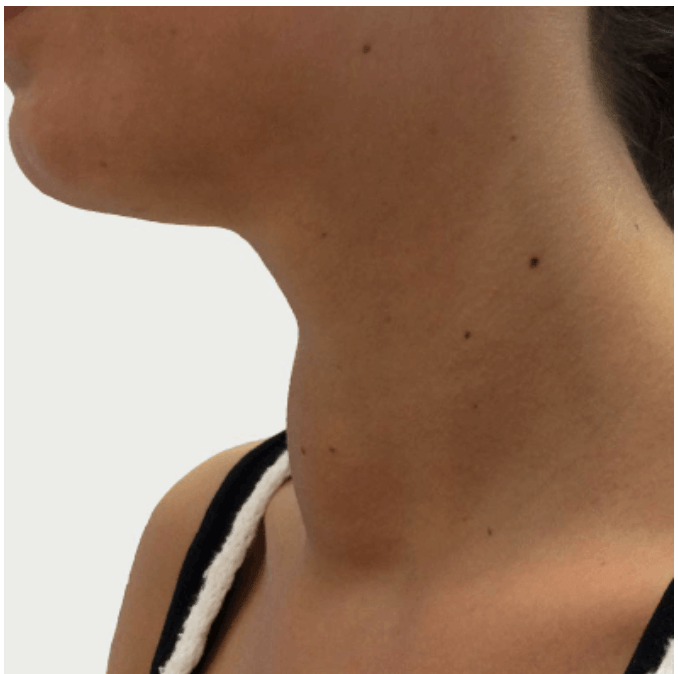
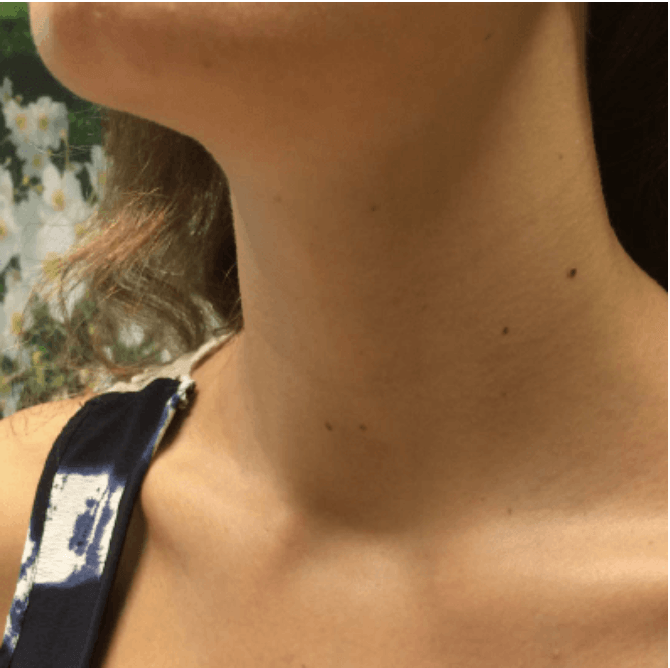
BEFORE / AFTER
RADIOFREQUENCY ABLATION PROCEDURE
RADIOFREQUENCY ABLATION THERAPY: FREQUENTLY ASKED QUESTIONS
Have more questions that we didn't answer here?
Schedule a Consultation Today
Little to No Scarring
This is a picture of a patient 1 month after receiving treatment via Radiofrequency Ablation. Scarring is almost non-existent.